Dortmund, 2nd August 2024
In most humans, every millilitre of blood contains more than 200 million thrombocytes (platelets). These smallest of blood cells can play an enormous role in the most common causes of death worldwide: ischaemic (coronary) heart disease and stroke. Thrombocytes can bind together in a flash, forming a thrombus (blood clot), which can plug a vessel and stop the flow of blood – this is how they can cause heart attacks and strokes. Proteins on the surface of the platelet cells are amongst others responsible for thrombogenesis. These proteins control activation of the thrombocytes – but the details of exactly how the proteins do this are still unclear. That is why ISAS researchers are working to decode the subtle changes that take place in the protein structure of these platelets. They want to identify the molecular markers that indicate thrombocyte activation so that, in future, medical experts will be able to detect and respond to a thrombosis before it even occurs
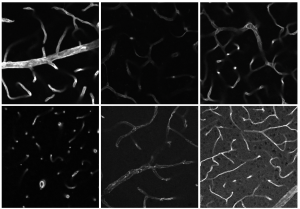
Thrombocytes, from the Ancient Greek θρόμβος for "clot", are flat and round, like a discus, for most of their existence. The body produces them in the bone marrow. The important role thrombocytes have to play in blood clotting has been known since the late 19th century: if a blood vessel is injured anywhere in the body, thrombocyte receptors detect this and cause platelets to stick together in that location. This produces a plug, or thrombus, which seals the blood vessel. However, if a clot like this forms away from a "leak", this creates thrombosis. Many people take medication every day in an effort to prevent this. One such drug is Aspirin® (acetylsalicylic acid), which reduces thrombocytes' ability to stick together. This medication therefore inhibits blood clotting and helps to prevent heart attacks and strokes, amongst other things.
Exhausted and sticky
Thrombocytes are able to alter their form dramatically and ad hoc, as when clotting the blood, but they can also change slowly and subtly – meaning they feature in many other processes in the body too. Platelets are involved in inflammatory processes, play a part in spreading metastases and respond to bacterial or viral pathogens (causative organisms) by forming thrombi, for example.
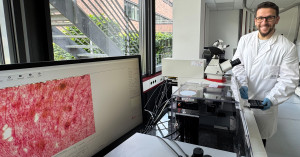
"We do not yet have any reliable biomarkers that can act as an early warning system for the various processes involving thrombocytes," says Prof Dr Albert Sickmann, Chair of ISAS's Board of Directors and an expert in clinical proteome research. Until now researchers worldwide have made do with cataloguing sub-populations of thrombocytes and giving them names like procoagulant, coated, exhausted or sticky.
Prof Dr Albert Sickmann's team carries out multi-omics analyses at ISAS.
© ISAS / Hannes Woidich
To establish which proteins are responsible for which particular behaviour of the platelets, researchers at ISAS conducted mass spectrometry analyses and identified 5500 proteins that are found, in varying constellations, in thrombocytes (thrombocyte proteome). They created a database containing information about every single one of these proteins. Together with their cooperation partners from University Hospital Essen, the ISAS researchers now want to perform extensive analyses to figure out how thrombocyte protein profiles differ between people with varying physical conditions and increasing age. "We really hope that this work will help us to better understand the mechanisms that cause diseases," says Prof Dr Tienush Rassaf, Director of the Department of Cardiology and Angiology at University Hospital Essen.

Prof Dr Tienush Rassaf is Director of the Department of Cardiology and Angiology at Essen University Hospital.
© Universitätsklinikum Essen
A database that's free to access all over the world
ISAS has many years of experience in analysing thrombocytes to fall back on. The researchers are currently investigating thrombocytes from a group of over a thousand people, some with heart conditions and some healthy controls. It is the world's biggest study into the thrombocyte proteome. A similar-sized analysis of the blood of stroke patients is set to follow. "In most patients we are able to quantitatively record 4000 to 4200 proteins, which is over 80 percent of the total proteins in a thrombocyte – in other words, the thrombocyte proteome," explains Sickmann. The biochemist expects that comparing these protein profiles will shed light on the details of how thrombocytes are activated. "We are also excited to see whether we will find any clues as to why one person suffers a stroke, while another has a heart attack," says Sickmann. Once they have completed their analyses, the ISAS researchers want to open up their thrombocyte proteome database so as many scientists as possible all over the world can access it for help in answering their medical questions.
Finding a handful of proteins amongst thousands
In their multi-omics analyses (see statement Dr Fiorella Solari down below), the researchers at ISAS manage with tiny sample volumes. To be more precise, ten samples of 10 millilitres of blood are enough to elucidate complex molecular mechanisms and identify patterns of biomolecular changes that are associated with activating or inhibiting platelets. In 2023 the team of researchers working with Sickmann summarised the possible methods for analysing thrombocytes in a review article in the journal Current Opinion in Chemical Biology. Alongside proteomics, these methods are transcriptomics, phosphoproteomics, N-terminomics, glycoproteomics and lipidomics. They conclude that integrating multi-omics technologies further will open up new perspectives for explaining molecular and biochemical processes, including with regard to thrombocyte activation.

Multi-omics: From proteomics to N-terminomics and transcriptomics
Omics technologies are molecular biological methods such as genomics, lipidomics, metabolomics or proteomics, which we researchers use to study biomolecules from tissue samples or blood, for example, at a global level. Since they cover multiple molecular levels, multi-omics technologies can provide results that give a full picture of a sample. Omics technologies are an important starting point in personalised medicine as they produce huge amounts of data, which shed light on disease processes and potential treatment approaches.
Proteomics is the analysis of the proteome, which is the entire set of all proteins in an organism; phosphoproteomics focuses on adding and removing phosphates as molecular switches for proteins; N-terminomics is a branch of proteomics that studies how proteins degrade; glycoproteomics concentrates on proteins that contain carbohydrates as a result of post-translational modifications;transcriptomics is the study of the relative frequency of RNA transcripts; lipidomics refers to the large-scale analysis of the entire set of lipids.
Dr Fiorella Solari is a research associate in the Proteomics research group
Reliable parameters for clinical diagnostics
The process of creating molecular profiles for inclusion in the thrombocyte proteome database is laborious. "We suspect that, out of thousands of proteins in a thrombocyte, only a handful need to change to affect a person's health. And because the differences between the proteins could be incredibly small, we must compare the blood of an enormous number of patients and healthy individuals in order to find them," explains Sickmann.
In the medium term the researchers hope to identify reliable parameters for conditions such as heart attacks or strokes with the help of protein profiles. Where possible, the findings from the analyses could also help patients whose blood clotting ability is impaired due to a genetic condition. This is the case with Glanzmann's thrombasthenia, for example, which affects one person in every million worldwide. In this disorder, patients' thrombocytes are missing a receptor, which means that platelets do not clump together as well as in a healthy person. If the condition remains undiagnosed it can be life-threatening, as patients can easily lose dangerous amounts of blood when undergoing only minor surgery.
(Ute Eberle)