Dortmund, 13th March 2024
Hepatitis B and C, but also a fatty liver caused by high alcohol consumption or being overweight, are the most common causes of cirrhosis of the liver. Diseases of the liver often take a gradual course and are frequently asymptomatic to begin with. But one thing is clear: the earlier cirrhosis of the liver is treated and complications are recognised, the higher the patients’ chances of survival. A new approach to diagnosing life-threatening deteriorations, such as infections and organ failure, at an early stage has been developed by ISAS immunologist Professor Dr Matthias Gunzer. The mobility of certain immune cells within the human body could help predict an imminent deterioration in a patient’s health.
When the human body is no longer able to compensate for the gradual failure of the liver, patients face an acute decompensation (AD) of the cirrhosis of the liver (see info box). This rapidly occurring complication arises from inflammatory reactions and defective immune responses. Some patients develop a sepsis (blood poisoning) or quickly suffer an acute-on-chronic liver failure (ACLF), which sees further organs such as the kidneys or brain fail too. As there are currently hardly any therapeutic options for ACLF, some patients die within days.
In the past, research has found that immunological and inflammatory mechanisms play a decisive role in how cirrhosis of the liver progresses. Severe dysregulation of the immune system is a consequence of cirrhosis of the liver and the reason that sufferers are highly susceptible to infections.
The life expectancy of patients with cirrhosis of the liver depends on whether and which disease-related complications occur and are identified at an early stage. “To date, we in the medical sector have had no way whatsoever to predict complications such as infections or organ failure. And that is a huge problem because it means we are always running the risk of being overtaken by events and losing patients,” says Prof Dr Christian Lange, head of the Liver Centre at the University Hospital of Munich. He explains: “To be able to act in time, for example, by administering antibiotics or even performing a liver transplant, we would have to find out as early as possible about a further deterioration in vital functions such as organ failure or infections. But such a marker was lacking to date.”

Prof Dr Christian Lange heads the Liver Centre at the University Hospital of Munich.
© bildwerkeins - paul walther
CIRRHOSIS OF THE LIVER
Although the liver is a vital organ, its central importance for the human body is often underestimated. It is not only responsible for detoxification and for digesting fat, but also for storing energy. While it’s true that the liver is the only organ capable of regenerating itself, this is, only possible up to a certain degree of damage. Cirrhosis of the liver constitutes one of the leading problems for the global health system and even in industrialised countries such as Germany it is not uncommon. With this disease, the liver tissue is increasingly destroyed and replaced by connective tissue. The tissue hardens, becomes scarred and shrinks as well, which is why the disease also has the colloquial name “shrunken liver”. The liver is then no longer able to fulfil its vital tasks at all or only incompletely.
The functional analysis of specific immune cells might be useful in monitoring the health of patients with cirrhosis of the liver and in detecting impending complications as early as possible. The blood stem cells in the bone marrow produce more neutrophil granulocytes as a reaction to infections (see info box), which then migrate in the direction of the source of infection. And it is precisely this migration that immunologist Prof Dr Matthias Gunzer has in his sights. He heads the Biospectroscopy department at ISAS and is Director of the Institute for Experimental Immunology and Imaging at University Hospital Essen. “For more than one hundred years, we have known that neutrophils move. And now we even know down to molecular detail how the immune cells do this and which proteins are responsible for this process inside the cells,” he explains.
In medical practice, this knowledge has to date remained unused, however; there is a lack of functional examinations of human blood. Depending on the clinical picture, practitioners may have a look at the number of immune cells, but they do not investigate whether they are functioning normally or not. This means that it is possible for the blood count to be in the normal range in terms of numbers – but the function of the neutrophils, such as their movement, is nevertheless impaired.

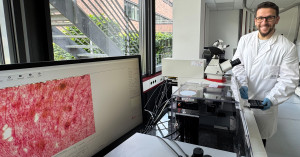
Prof Dr Matthias Gunzer heads the Department of Biospectroscopy and the Biofluorescence research group at ISAS. He is Director of the Institute for Experimental Immunology and Imaging at the University Hospital Essen.
© ISAS / Hannes Woidich
NEUTROPHIL GRANULOCYTES
These immune cells perform important tasks in the human body. Neutrophil granulocytes are primarily responsible for being the first line of defence against infectious agents such as bacteria and fungi. They are able, for example, to identify and kill or eat up micro-organisms and other structures that are foreign to the body.
Migration of the neutrophil granulocytes as a potential marker
Gunzer has developed an assay (laboratory test) that analyses the migration behaviour of the neutrophils. The findings could permit conclusions to be drawn about a patient’s health and act as markers to facilitate the early detection of complications. In brief: routine and regular measurement of the movement of neutrophils could act as an early warning system for medical professionals.
This was how the idea arose of Lange and Gunzer collaborating. The big question was this: can the movement behaviour of the neutrophil granulocytes predict whether the health of patients with cirrhosis of the liver will deteriorate within a few days or weeks? Lange and Gunzer decided to deploy their teams to use the standardised migration assay to characterise how the neutrophils migrate in the blood of sufferers.
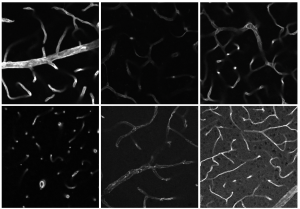
The researchers used immunomagnetic separation to isolate the neutrophils from the blood of 125 patients with cirrhosis of the liver at the Liver Centre at different stages of severity of the disease and from the blood of 24 healthy individuals. In the experiment, the researchers added three different active agents (the chemotactic formyl peptide f-Met-Leu-Phe and the chemokines CXCL1 and CXCL8), which are known to trigger the migration of the neutrophils. With a cell culture microscope, they took images of the neutrophils every eight seconds for one hour. The researchers then combined these images to make videos that allowed them to automatically evaluate the movement of the cells over the course of time. Furthermore, they used flow cytometry (see info box) to examine the relationship between the neutrophil migration and the expression of chemokine receptors and activation markers on neutrophils.
FLOW CYTOMETRY
With the help of a flow cytometer, it is possible to determine, for example, molecules such as proteins on the surface of and inside individual cells quantitatively and at high speed. In this respect, the device follows a physical-chemical principle: a stream of liquid transports cells. They flow quickly past a laser beam and are analysed by means of the scatter of visible light or by fluorescence. Over and above this, the cells influence the laser light depending on their size, the structure of their membrane or the content of intracellular structures.
Different migration patterns are apparent
The study ultimately succeeded in actually discovering special migration patterns amongst the neutrophils of patients with cirrhosis of the liver who have a high risk of developing complications. The researchers under Lange and Gunzer therefore came to the conclusion that a large proportion of immobile neutrophils and a high average velocity of the moving neutrophils are particularly characteristic of a high risk of developing a sepsis or an ACLF, or even dying, over the next seven to 30 days.
The new method of analysing neutrophils has ultimately shown that it is possible to regularly observe the behaviour of these immune cells in patients with cirrhosis of the liver and to establish whether pathological migration patterns are developing. But until the examination can become standard clinical practice for sufferers, the experimental approach will have to be simplified and automated using machine-based algorithms so that the blood test can be performed quickly and with little intervention by staff on a routine basis. “Transposing this procedure into clinical practice would make it possible for the first time to detect infections and organ failure at an early stage in patients with cirrhosis of the liver. This would enable us as medical practitioners to put therapeutic measures in place at an early stage and to save the lives of sufferers,” says Lange.
Mobility test can also be used with other disease profiles
Incidentally, the mobility test of neutrophil granulocytes is not restricted to use in patients with cirrhosis of the liver. Gunzer: “As far back as 2018 we were able to demonstrate that the severity of a preliminary stage of leukaemia can be evidenced through the migration behaviour of the neutrophil granulocytes. Early detection in diseases other than leukaemia and cirrhosis of the liver would also be conceivable.”
(Christine Kirchhoff)
Article Recommendation
Langer, M.-M., Sichelschmidt, S., Bauschen, A., Bornemann, L., Guckenbiehl, S., Gunzer, M., Lange, C.M. (2022). Pathological neutrophil migration predicts adverse outcomes in hospitalized patients with liver cirrhosis. Liver Inernational, 43(4), 896-905. https://doi.org/10.1111/liv.15486.